The Injury
Plantar Fasciitis (heel-spur syndrome) is a common problem. It starts as a dull intermittent pain in the heel which may progress to a sharp persistent pain. Classically, it is worse in the morning with the first few steps, after sitting, after standing or walking, and at the beginning of sporting activity.
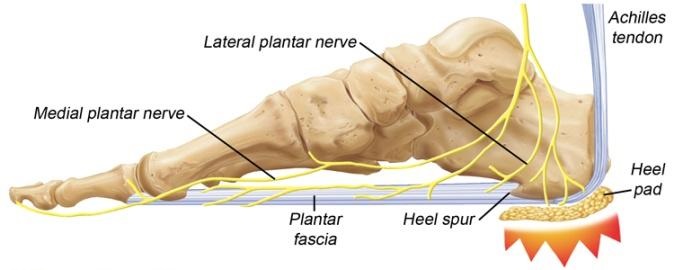
The plantar fascia is a thick fibrous material on the bottom of the foot. It is attached to the heel bone (calcaneus), fans forward towards the toe, and acts like a bowstring to maintain the arch in the foot.
A problem may occur when part of this inflexible fascia is repeatedly placed under tension, as in running. Tension causes an overload that produces an inflammation usually at the point where the fascia is attached to the heel bone. The result is pain. Plantar fascia injury may also occur at midsole or near the toes. Since it is difficult to rest the foot, the problem gradually becomes worse because the condition is aggravated with every step.
The inflammatory reaction at the heel bone may produce spike-like projections of new bone called heel-spurs. They are sometimes shown on X-rays. The exact relationship between heel spurs and plantar fasciitis is poorly understood. The heel spurs do not cause the heel pain and they are not the initial cause of the problem. Indeed some people may have heel spurs found incidentally on X-rays but may be completely pain free.
Treatment
Improvement may take longer than expected, especially if the condition has been present for a long time. During recovery, loss of excess weight, good shoes and sedentary activities all help the injury to heal. You should return to full activity gradually.
Rest: Use pain as your guide. If your foot is too painful, rest it.
Ice: Ice the sore area for 30-60 minutes several times a day to reduce the inflammation. Apply a plastic bag of crushed ice over a towel. You should also ice the sore area for 15 minutes after activity.
Medication: If your condition has developed recently, anti-inflammatory/ analgesic medication (in tablet form), coupled with heel pads may be all that is necessary to relieve pain and reduce inflammation. If no pain relief has occurred after two or three months, however, an injection of either cortisone and/ or local anaesthetic directly into the tender area may be considered.
Physiotherapy: The initial objective of physiotherapy (when needed) is to decrease the inflammation. Later, the small muscles of the foot can be strengthened to support the weakened plantar fascia.
Heel Pads: A heel pad of felt, sponge or a newer synthetic material can help to spread, equalize and absorb the shock as your heel lands, thus easing the pressure on the planter fascia.
Shoes: Poorly fitting shoes can cause plantar fasciitis. The best type of shoe to wear is a good running shoe (jogger/trainer) with excellent support. The shoe that fits best should be chosen. Experiment with your athletic shoes to find a pair that is comfortable and gives you fewer symptoms.
Orthoses: Orthoses are shoe inserts that Dr Pradeep Moonot may prescribe if necessary.
Taping: Taping your foot to maintain the arch may benefit some people as this can take some of the pressure off the plantar fascia.
Night Splints: These are plastic splints that keep the foot stretched and the ankle at right-angles when you are asleep. This maintains the tension in the plantar fascia and may help to alleviate some early morning symptoms during the first few steps of the day.
Surgery: Surgery is rarely required for plantar fasciitis. It would be considered treatment if the pain is still incapacitating after at least 12 months of treatment. When needed, surgery involves release of the plantar fascia and release of a small nerve.
Sports
Plantar fascia can be aggravated by all weight bearing sports. Any sport where the foot lands repeatedly, such as jogging or running can aggravate the problem. To maintain cardiovascular fitness, weight bearing sports can be temporarily replaced by non weight bearing sports (like swimming, cycling). Weight training can be used to maintain leg strength. When recovering from plantar fasciitis, return to sports activities slowly. If you have a lot of pain either during the activity or the following morning, you are doing too much.
Exercise
Stretches: Stand at arms’ length from a counter or table with your back knee locked and your front knee bent. Slowly lean towards the table, pressing forward until a moderate stretch is felt in the calf muscles of your straight leg. Hold 10 seconds. Keeping both your heels on the floor, bend the knee of your straight leg until a moderate stretch is felt in your Achilles tendon. (Tendons attach muscles to bones; the Achilles tendon attaches the muscles of the calf to the heel bone). Hold 10 seconds. You should feel a moderate pull in your muscles and tendon, but no pain. Change legs and stretch the other leg.
Repeat 10 times, 3 times a day.
Medical Team
DR. PRADEEP MONOOT
MBBS (Bom), MS (Ortho)(Bom), DNB (Orth), MRCS (UK), FRCS (Ortho) (UK)